The Origins of Eczema
What came first, the chicken or the egg?
The eczema journey is different for each child and consists of a lot of trial and error. As frustrating as it is to hear this, it will make more sense the deeper we dive into the origins of eczema. In fact, one of the most trivial parts of the entire eczema journey is determining and understanding the origins of your child’s eczema. This is no easy feat as there are different theories on where eczema originates and it can be quite confusing. And if that was not hard enough… neither is wrong. Dubbed the million dollar question. Which came fist, the chicken or the egg. Does eczema start in the skin? the internal organs such as the gut? or is it the respiratory tract? Before we can understand the origin theories, we need to start with the basics: defining eczema and inflammation.
What is Eczema?
The most common form of eczema is called atopic dermatitis (AD). The words eczema and AD are often used interchangeably. The American Academy of Dermatology (AAD) describes AD as a complex skin disease triggered by environmental factors in genetically susceptible individuals. It is indeed a complex interaction of genetic, immune, and environmental factors. You will find that eczema is really a web of dysfunctional barriers, impaired interactions, and overactive immune responses. In a nutshell: people with eczema tend to have an overactive immune system that responds to irritants by producing inflammation. The immune system is stuck in the “on” position. Furthermore, eczema is considered an “inflammatory skin disease”. Do not let the “skin” in the name fool you. Remember, there are different theories on the origins of eczema and neither of them are wrong. Keep an open mind- we will discuss ALL of it!
Parents are often told that the prognosis of their child’s eczema depends on the severity, frequency, and whether they are genetically predisposed to this skin disease. The next step involves identifying potential triggers, avoiding them at all costs, and often receiving a prescription to help combat the flare. Despite well intentions, these kiddos often get stuck in what we call an “itch and scratch cycle” of eczema. I really feel we can all do a much better job of managing eczema if we understood the pathogenesis better. Now lets discuss what inflammation is, as this is the basis of eczema- an inflammatory skin disease. Notice I did not emphasize “skin”.
What is Inflammation?
When we think of inflammation, red, swollen, hot, and painful come to mind. Typically due to infection or injury. As it pertains to skin, this is caused by inflammatory immune cells (cytokines) coming to the surface of the skin. Triggers of inflammation in atopic dermatitis include family history of allergic conditions such as asthma, eczema, food allergies in one or more parents, impaired skin barrier, nervous system imbalances, immune dysfunction, stress, excessive hygiene (too sterile leading to more exaggerated immune responses), and environmental pollution (i.e. car exhaust/wildfire pollution).
While both psoriasis and eczema are inflammatory diseases, they have different inflammatory molecules/cytokines specific to the disease. For example, psoriasis is largely driven by Th17 T-cells and associated IL-17 activation, while AD has a strong Th2 component associated with IL-4 and IL-13 overproduction. Both diseases have activation of the Th22 T-cells and Th1 pathways with increased IL-22 and IFNy production (now that is a mouthful!). Inflammation can be localized or body wide (systemic). Eczema can actually be both due to a defective skin barrier (known as Outside-in theory). Think of a broken fence that provides no barrier to the escape of chickens (since we are on the topic of chicken or egg). When a skin’s barrier is “broken”, foreign antigens (allergens such as dust mites, irritants, and microbes) can enter the “leaky skin” and provoke an immunological response both on the skin and inside the body. This is why eczema is often associated with other allergic disorders.
Allergic Inflammation
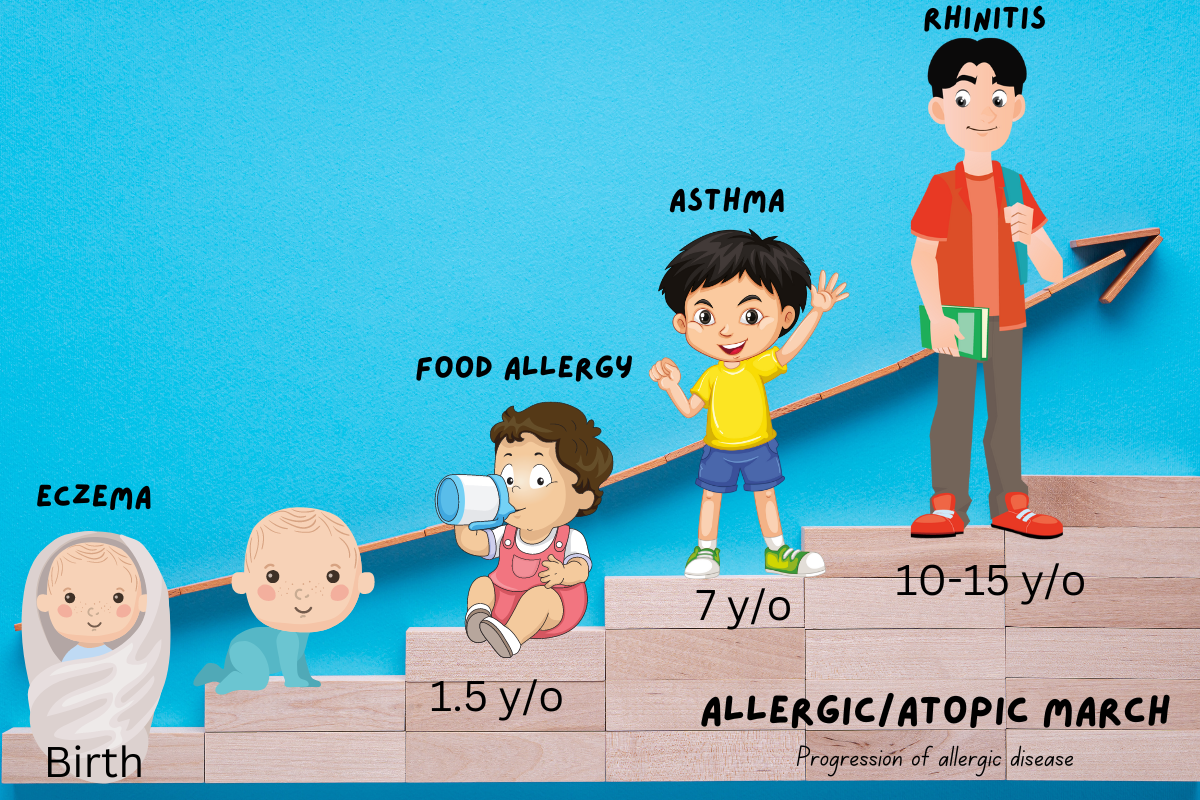
Many of those living with eczema have gone through something called the atopic/allergic march. The Outside-in theory explains the root pathogenesis in this subset of patients. Skin barrier disruption results in increased skin AND body wide (systemic) Th2 response (i.e. IL-4/13). In other words, inflammatory Th2 cells are triggered by an impaired skin barrier (more on this below) resulting in Th2 dominance (too much Th2). This Th1/Th2 disbalance leads to the development of inflammatory dermatitis (inflammation of the skin) AND allergic diseases such as food allergies, asthma, and hay fever. Basically, the foreign antigens that have “gotten through the fence” so to speak, stimulate production of specific antibodies called immunoglobulin-E (Ig-E). Ig-E binds to the foreign antigens, which causes mast cells to release their stores of histamine, which then triggers itchy skin, constriction of bronchial tubes in the lungs, etc. I like to think of mast cells as giant piñatas floating around the body ready to explode and spill candy (histamine).
The atopic/allergic march typically occurs in a sequential manner starting with eczema during infancy. This same child, around age 1.5-2 years old may develop food allergies, and around school age develop asthma. The last of the atopic/allergic march component occurs in middle or even high school age children as allergic rhinitis or hay fever (seasonal allergies). One in three children with AD will develop asthma or allergic rhinitis like this, with severity of AD correlating with this progression (the more severe their eczema, the more likely they will proceed down the atopic/allergic march). Those with family history of allergic diseases such as asthma, eczema, and food allergies in 1 or more parents are also at higher risk of progressing through this atopic/allergic march.
Skin Barrier Disruption
Recently, mutations and polymophisms of inflammatory genes have been linked to AD (i.e. single nucleotide polymorphisms (SNPs) of IL4RA, CD14, SPINK5, RANTES, IL-4, IL-13). Nearly 30% of eczema patients have mutations in the gene for filaggrin (part of inside-out theory). Filaggrin is a protein that helps maintain skin structure by binding keratin filaments together to strengthen and flatten skin cells. If you don’t have enough functioning filaggrin, skin cells can lose moisture, shrink, and develop gaps (holes in the walls of your skin aka “leaky skin”). With loss of moisture, skin becomes dry and itchy, leading to scratching/rubbing, which can further weaken the skin barrier, allowing allergens, irritants, and microbes to go in, causing even more water to go out, making skin even more itchy, dry, and prone to infection. It is important to note that people without filaggrin mutations can also have reduced filaggrin gene expression due to immune dysregulation. How does filaggrin tie-in with immune dysregulation? As discussed above, this skin disruption results in increased cutaneous (skin) and systemic Th2 responses, cytokines such as IL-4 and IL-13 (I am sure you have noticed that these are major mediators of Th2 cell response in eczema) are increased, which downregulates genes involved in filaggrin production/ faulty versions of this protein, leading to disrupted skin barrier, even in people without a filaggrin genetic mutation. It is also assumed that environmental factors such as temperature and humidity can affect filaggrin production. This is why moisturizing on repeat is so crucial! Another HUGE takeaway here as this is a common misconception about eczema… itchiness does not always mean histamine overload! Skin barrier dysfunction + immune cell dysfunction+ sensitization of sensory nerves= “itch and scratch cycle” of eczema.
Itchy Skin, Sensory Nerves, & Immune System
How does sensitization (responding to stimuli in a sensitive/exaggerated manner) of sensory nerves and the itch and scratch cycle of eczema occur? Loss of moisture results in dry itchy skin which often leads to scratching = disruption of the skin barrier. A cytokine located on epithelial cells of the skin called the Thymic stromal lymphopoietin (TSLP) is expressed in response to “danger signals” due to skin injury. Interestingly, moisturizer application results in reduced skin TSLP levels! As TSLP production is increased, this provokes the type 2 inflammatory immunological response (Th2 dominance) both on the skin AND inside the body. The Th2 cells secrete immune cells, cytokines IL-4, IL-13, and IL-31 (another cytokine elevated in AD and associated with itch) which stimulates sensory cutaneous (skin) neurons involved in the induction of itch. The immune cells stimulation of sensory nerves creates a positive feed back loop- the brain perceives an itch signal (sensory nerve dysfunction), the brain tells hand to scratch the skin even if small trigger (due to strong perception to itch stimulus), and the itch and scratch cycle begins further aggravating dermatitis (skin inflammation). We often forget that the immune system works with nerves in the skin. Those topical remedies can really come in handy by breaking the cycle of itch and scratch, whilst working on addressing dysfunctional barriers, impaired interactions, and overactive immune responses. Furthermore, skin neuropeptides such as substance P, vasoactive intestinal peptide (VIP- only Th2 cells produce this), nerve growth factor, and acetyhlcholine also modify the functions of immunoactivity cells in the skin. NGF and NPs modulate the allergic response in AD. Still lots of research to be done when it comes to the role of NPs and NFG in AD.
In summary: the vicious cycle of scratching behavior of the skin causes physical damage to skin barrier which causes leaky skin leading to the the entrance of allergens, microbes, and irritants causing more inflammation AND imbalance of the skin microbiome & beyond (further exacerbating the itch and scratch cycle of eczema). Now its time to move on to main question at hand: the chicken or the egg?
The Two Theories
The million dollar question: Inside-out or outside-in?
Although all of these immunologic features are well established in AD, controversy still remains as to whether AD is caused by systemic inflammation triggering barrier dysfunction (the “inside-out” hypothesis) or from the epidermal skin barrier disruption triggering immunologic imbalance (the “outside-in” hypothesis).
Inside Out theory: starts inside (internal organs such as the gut or lung) and then goes outside (skin).
Immune dysregulation
Cascade of (systemic) inflammation
Triggering barrier dysfunction.
The functions of the intestinal/ barrier is to make sure that what belongs in the gut stays in the gut. Exposure to barrier damaging agents such as medications, stress, toxins, bacteria, food particles can all cause damage to intestinal cells. The lining of the gastrointestinal tract is a simple columnar epithelium, or only one cell thick. Why is it only one cell thick? To accommodate the exchange of nutrients and water! When this simple barrier fails due to inflammation “leaky gut”, leading to colonization of opportunistic pathogens, decreased biodiversity (microbial dysbiosis), endotoxins produced by certain species of gut bacteria and antigens (food allergens and irritants) can enter the blood stream (translocation of microbiota and antigens) and provoke an immune response to antigens…. leading to immune dysregulation (immune system not working properly - specifically T helper type 1 (Th1) and T helper type 2 (Th2). This causes a cascade of inflammation with the immune particles diffusing through the blood stream and ending up in the skin, causing inflammation, and barrier dysfunction “leaky skin”.
Outside in theory: starts outside (skin) and then goes inside (internal organs such as the gut or lung).
Epidermal skin barrier disruption, trans-epidermal water loss, reduced skin hydration
Penetration of antigens- allergens, irritants, microbes
Triggering immunologic imbalance due to translocation of microbiota to sub-epithelial areas (other areas of body below the skin surface!)
Langerhans cells initiating inflammation
The Skin-Lung-Gut Crosstalk
We have established that medications, stress, toxins, bacteria, and food particles can cause damage to the intestinal, lung, or skin cells. These particles diffuse through the blood stream from point A to point B. Does the enticing event start from these particles damaging intestinal cells then diffusing through the blood stream and ending up in the skin causing inflammation OR the same particles causing a skin barrier defect then diffusing into bloodstream before reaching cells in the lungs/gut causing food allergies and asthma? The chicken or the egg. Well…. it can be both ways! Neither is wrong or perfect. It is likely that both the inside-out and outside-in hypotheses are true in different subsets of patients.
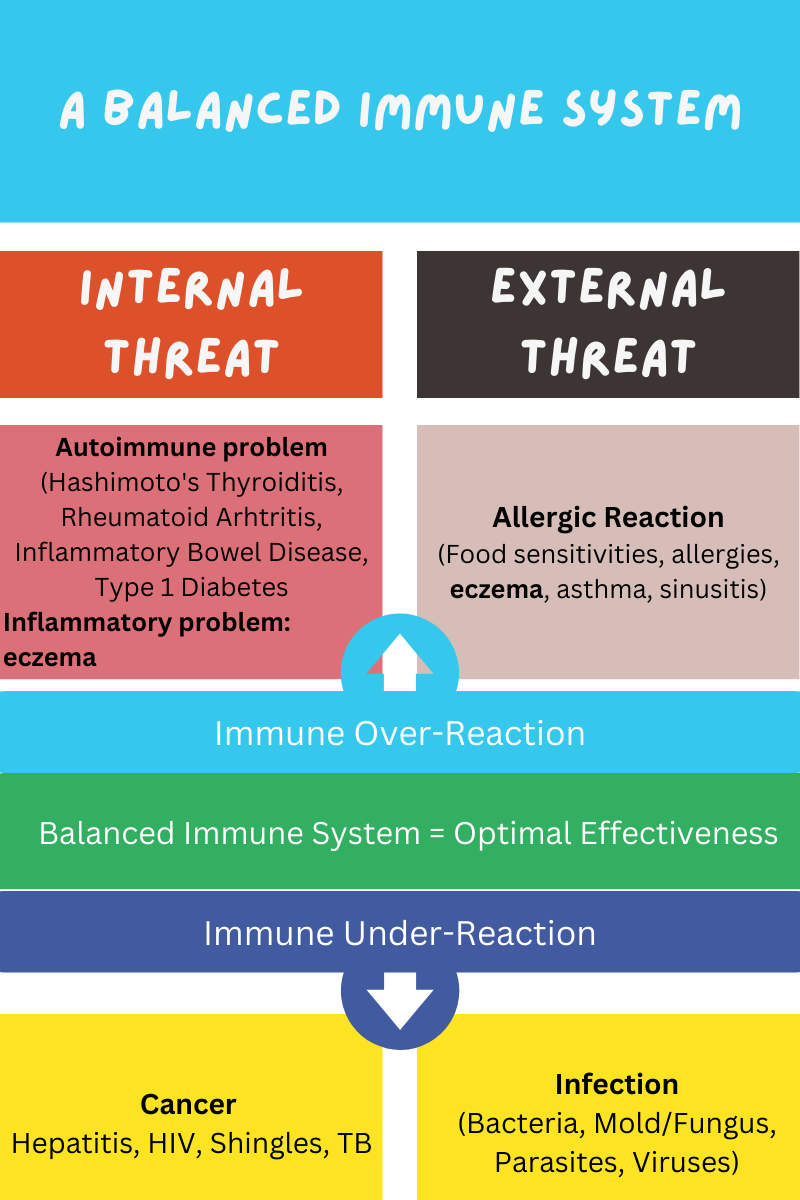
A Balanced Immune System
Regardless of whether the chicken came before the egg or vice versa, a balanced immune system (Th1/Th2) is very important for optimal effectiveness and to decrease unwanted inflammation.
Immune over-reaction from internal threats can lead to autoimmune/inflammatory problems (eczema included since it lies in the middle of the sandwich). Immune over-reaction can also be due to external threat causing allergic reaction (food sensitivities, eczema, asthma, etc). If immune system is under-reacting, body cannot fight cancers and other infections. This is why it is important not to suppress immune system too much when treating conditions such as eczema. The key is to modulate immune system so it stays balanced. An imbalance in EITHER the skin or gut microbes often affects the other. Eczema is a MULTIFACTORIAL INFLAMMATORY DISORDER.
Dysbiosis
Dysbiosis means an imbalance in the microbiome = too few beneficial bacteria, overgrowth of pathogenic bacteria (including fungi and viruses) and not enough good native bacteria (aka commensal bacteria). We discussed that eczema is an inflammatory skin disease. It actually falls in the middle of the spectrum between skin infections and autoimmune disease. Think of a peanut butter and jelly sandwich (I made a visual to help!). One slice of bread has bacteria (skin infection) and the second slice has abnormal immune cells on it (autoimmune skin disease).
Skin infections = overabundance of “bad bacteria” colonizing the skin (staphylococcus aureus and its toxins alpha + delta)
Autoimmune skin disease (i.e. lupus, psoriasis)= too much abnormal immune cells on the skin
Inflammatory skin diseases (eczema) lies in the middle of the sandwich (the PB&J ) caused by abnormal immune cells AND abnormal microbiota on the skin.
Skin Microbiota-Immune Crosstalk
Did you know our skin microbiome talks to our immune cells?? The skin microbiome serves as an instructor for our immune cells. This is how our immune system knows what is part of self and what is foreign. If this crosstalk between the skin microbiome and immune cells is impaired, and the immune system does not recognize something that is actually bad/foreign, this would lead to infection. Similarly, if the crosstalk is impaired, and the immune system thinks something that is self as foreign and attacks it, this would lead to an autoimmune condition.
Are We Too Sterile?
Excessive hygiene may also be a contributing factor to an exaggerated immune response due to the skin microbiota-immune cross talk hypothesis. If the skin microbiome is too sterile, there are no instructors to teach our immune cells how to respond appropriately resulting in allergic diseases such as AD.
Studies examining the skin of individuals with AD have found an overabundance of bad bacteria (staphylococcus aureus and its toxins alpha + delta) and not enough good (commensal/native) bacteria such as staph. epidermidis, Corynebacterium, Propionibacterium. A study evaluating the relationship between skin microbiota and disease progression found when AD is in remission, the skin microbiome diversity is high (baseline) but when disease is about to flare (pre-flare), the proportion of staphylococcus increases and the disease severity then follows this increase in staph aureus. The study shows a close time association with the change in skin microbiome and AD flare. Interestingly, as they treated the disease, there was resolution of the disease severity AND the skin microbiome diversity increased back to baseline. The takeaway from this study is that in order to treat AD, restoring skin microbiome is important.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3337431/
As you can see, there is a deep interrelation of immune activation, “leaky skin”, altered skin microbiome i.e. bacteria such as staph aureous toxins which damage the skin barrier and trigger cytokines (IL 4, IL 13, IL 31)
Until we can determine the genomic or triggering events in each individual, we should approach childhood eczema from the inside-out through appropriate treatment of systemic inflammation and immune dysregulation, and from the outside-in with skin barrier treatment and prevention.
Resources
https://nationaleczema.org/webinar-gtf-inflammation/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3337431/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5467082/#:~:text=Type%202%20inflammation%20describes%20an,titers%20and%20eosinophilia%20(23).
https://pubmed.ncbi.nlm.nih.gov/20616938/
https://onlinelibrary.wiley.com/doi/full/10.1111/jdv.14891
Next topic: How to Calm Inflammation in Eczema